Chronic Knee Pain and Dementia – New Study
Jayney Goddard MSc, FCMA, FRSPH, Lic.LCCH, Dip.ACH. President: The Complementary Medical Association
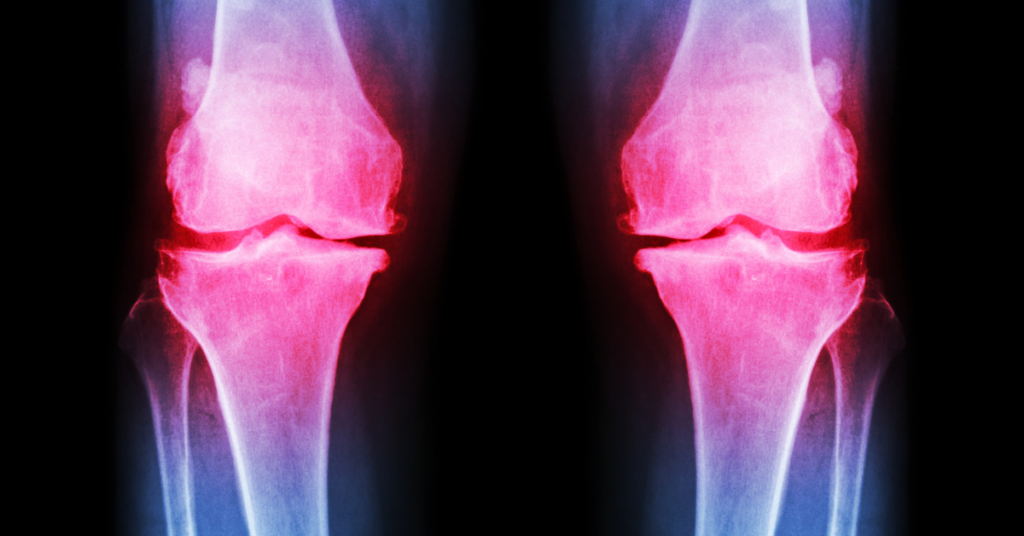
Jayney Goddard discusses an exciting new study that links chronic pain (CP), including knee osteoarthritis, to accelerated brain biological ageing – and the development of dementia.
Researchers in China and the US have discovered that chronic musculoskeletal pain (CMP) could be linked to a higher risk of brain aging and dementia.
- People with knee osteoarthritis were found to have more rapid brain aging than people without it.
- A genetic link between inflammation and brain function may point toward a way to predict cognitive decline.
- This research is directly relevant to those of us in complementary and integrative medicine (CIM) as our disciplines and lifestyle medicine approaches have so much to offer in reducing the dangerous health burden of chronic inflammation.
CMP may contribute to a higher risk of cognitive decline, according to a new study by scientists from the US and China.
The study, published in Nature Mental Health, examined the MRI data from more than 9,000 people in the UK and discovered a connection between knee osteoarthritis (KOA) and accelerated brain aging.
With slightly less than half of the global population experiencing CMP, the study provides a window for researchers into how inflammation and cognitive function can be linked and studied in the future. CMP’s role in accelerated cognitive decline has not been extensively studied, but many older adults who experience it are at greater risk for dementia.
Researchers developed a comparative model using structural MRI data that allowed them to examine the differences between brain age and chronological age.
They found that people with KOA had much more rapid brain aging than those without it.
How does chronic musculoskeletal pain affect the brain?
Inflammation in the body has been seen as a contributing factor to neuro-physiological ailments, including depression, Alzheimer’s, Parkinson’s disease, traumatic brain injury (TBI), Amyotrophic lateral sclerosis (ALS), Gulf War Illness, myalgic encephalomyelitis (ME), and chronic fatigue syndrome (CFS).
It is believed that inflammation and chronic pain can interrupt and alter the brain’s processing patterns, so that chronic inflammation, e.g., knee osteoarthritis or chronic musculoskeletal pain are then associated with changes in the central nervous system. This causes neuroplastic responses, which lead to changes in the structure and function of the brain.
Chronic pain has significant implications for compromised cerebral structure and function – and this is due to changes in the ways in which pain is processed and this leads to disrupted cognitive functions, particularly with respect to the prefrontal cortex activity and architecture.
Chronic, not acute, inflammation is the issue
The inflammation that occurs as a result of acute pain can become chronic if not properly addressed, however, acute injury only to one particular area is unlikely to cause cognitive decline.
Linking chronic pain and cognitive decline
The new study suggests that the gene SLC39A8T, which is expressed in microglial cells and astrocytes, is the connection between KOA and cognitive decline. SLC39A8 encodes the protein ZIP8, which transports essential metals like ferrum, manganese, and zinc, and the nonessential neurotoxic metal cadmium.
A variety of factors, including genetic mutations, may also affect the transport and uptake of essential metals to the mitochondria, particularly manganese, which seems to be essential for the health and function of brain cells. It is important to note, however, that excess metal exposure or other toxic contaminants (food borne, environmental, etc.) can have major negative side effects systemically and upon brain health.
There are a number of other illnesses and clinical disorders seen in virtually every organ, tissue, and cell type as a result of CMP. These include developmental and congenital disorders, effects upon immune system function, cardiovascular compromise, kidney, lung, liver, coagulation system impairment, central nervous system, musculoskeletal, eye, and gastrointestinal tract conditions.
The researchers who developed this study believe that it should provoke further understanding of the links between CMP and cognitive decline, but also of the wider array of problems that can arise from the gene’s imbalance.
Traits with which SLC39A8-deficiency variants are currently associated include Mn2+-deficient hypoglycosylation; numerous birth defects; decreased serum high-density lipoprotein-cholesterol levels; increased body mass index; greater risk of coronary artery disease, hypotension, cardiovascular death, and Parkinson’s disease, among many others.
The role of complementary and integrative medicine – a way forward
As always, more work needs to be done to discern whether other forms of chronic pain affect brain structure and function, but this significant breakthrough is relevant to complementary medical practitioners as we have such a wide variety of ways of supporting our clients with chronic inflammation reduction using lifestyle approaches and relevant disciplines, including acupuncture, nutrition, massage and other bodywork / physical ‘hands-on’ therapies, homeopathy, herbalism, and mind / body approaches including hypnosis, mindfulness, and meditation. Naturally, the important roles of socialisation, kindness, gratitude and having a sense of purpose in one’s life (Ikigai), must also be considered as effective chronic inflammation mediators.
References
Zhao L, Liu J, Zhao W. et al. Morphological and genetic decoding shows heterogeneous patterns of brain aging in chronic musculoskeletal pain. Nat. Mental Health 2, 435–49 (2024). https://doi.org/10.1038/s44220-024-00223-3
(See also our articles The Effect of Lifestyle on Cognitive Impairment and Alzheimer’s Disease and Women – Disturbing Gender Bias and Neglect)